CLeAR supported long-term care homes in BC to provide person-centred care for residents with the behavioural and psychological symptoms of dementia (BPSD).
Clear was a clinical quality improvement initiative guided by Choosing Wisely’s recommendation on using antipsychotic medications to treat BPSD in cases where nonpharmacologic measures have failed, and where the symptoms either cause significant suffering, distress and/or pose an imminent threat to the patient or others.
Wave 3 supported care homes across the province whose use of antipsychotics (without a diagnosis of psychosis) is higher than the BC average of 25%. This included both affiliated and health authority owned-and-operated care homes and represents the most care homes to ever participate in Clear.
Featured CLeAR Resources
CLEAR Wave 3 Technical Report
CLEAR Wave 3 Summary Report
CLeAR Wave 2 – Final Evaluation Report
CLeAR Wave 1 – Final Report
CLeAR
Clear is supporting long-term care homes to carry out effective behavioural care planning and management that will lead to a reduction in the number of their residents who are prescribed antipsychotic medications
Interested in getting an idea of what has been happening in BC addressing antipsychotics in long-term care? Have a look at this BCCPA report: A Pathway to Ensuring the Appropriate Use of Antipsychotics in Continuing Care.
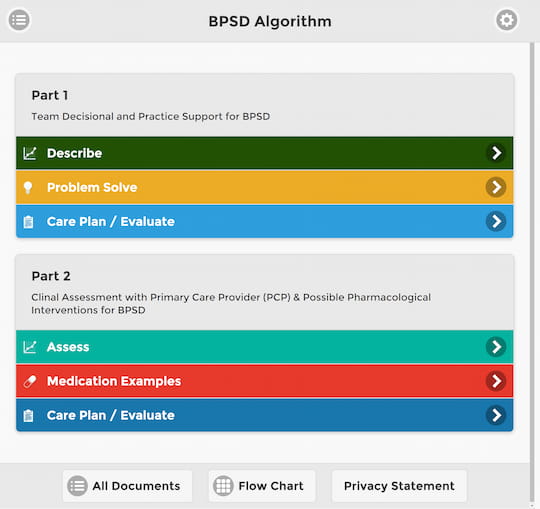
The CLeAR Approach
The following milestones provide a practical “roadmap” for the improvement journey. These milestones build upon themselves as the work progresses with some more focused on “Getting Started” and others on “Rolling Out the Work.”
The goal of the milestones is to develop an effective approach to behavioural care planning and management that will support the needs of the residents, while fostering the appropriate use of antipsychotic medication. High-impact changes and resources for each milestone have been identified below that provide further direction for this work.